Most cancer deaths are caused by metastatic tumors, which break free from the original cancer site and spread throughout the body. For that to happen, cancer cells must undergo many genetic and physical changes. Now, MIT researchers have developed a way to study three key physical properties of cancer cells — their mass, stiffness and friction — on a large scale.
Using this system, the researchers have analyzed how changes in those traits may allow cancer cells to migrate to new sites: Scientists have previously observed that cell lines with higher metastatic potential are generally more deformable, but the MIT team found that decreased friction also appears to help cancer cells traverse narrow channels, suggesting that friction may play a role in the ability of cancer cells to travel in blood vessels and reach new tumor sites.
“Our measurements provide an additional perspective on cell properties that may complement genomic and proteomic approaches,” says Sangwon Byun, an MIT postdoc and lead author of a paper describing the findings in the Proceedings of the National Academy of Sciences the week of April 22.
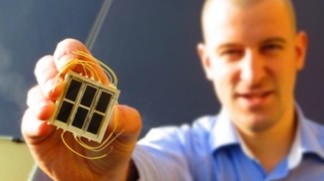
The system that Byun and colleagues used to study the cancer cells is based on a device previously developed by Scott Manalis, a member of MIT's Koch Institute for Integrative Cancer Research and an MIT professor of biological engineering. Manalis, the senior author of the PNAS paper, has previously demonstrated that this system, known as a suspended microchannel resonator (SMR), can very accurately measure the mass and density of individual cells.
The new MIT system is “probably the world’s most sensitive instrument for measuring a number of different biophysical properties of individual cells,” says Mehmet Toner, a professor of biomedical engineering at Massachusetts General Hospital and Harvard Medical School who was not part of the research team. “It’s very important to know whether metastatic cells have biophysical properties different than normal or nonmetastatic cancer cells, allowing them to go through narrow spaces.”
“When you use a specific marker to look for these cells, you find the cells that you’re looking for, but you may be missing a whole population of cells,” says Josephine Shaw, an MIT graduate student and a co-author of the paper. “It’s possible that by using a more holistic and physical approach, we may be able to find certain cells that we wouldn’t be able to find molecularly, because we wouldn’t be able to guess ahead of time what these cells would be expressing.”
Other authors of the paper are MIT postdoc Sungmin Son; Stanford University postdoc Dario Amodei; MIT grad students Nathan Cermak, Joon Ho Kang and Vivian Hecht; former MIT postdoc Monte Winslow; Tyler Jacks, the David H. Koch Professor of Biology at MIT and director of the Koch Institute; and Parag Mallick, an assistant professor of radiology at Stanford.
The research was funded by the National Cancer Institute, through MIT’s Physical Sciences Oncology Center and Stanford’s Center for Cancer Nanotechnology Excellence and Translation, and Stand Up to Cancer.