Inspired by a chemical that fungi secrete to defend their territory, MIT chemists have synthesized and tested several dozen compounds that may hold promise as potential cancer drugs.
A few years ago, MIT researchers led by associate professor of chemistry Mohammad Movassaghi became the first to chemically synthesize 11,11’-dideoxyverticillin, a highly complex fungal compound that has shown anti-cancer activity in previous studies.
In the new study, recently published online in the journal Chemical Science, Movassaghi and colleagues at MIT and the University of Illinois at Urbana-Champaign (UIUC) designed and tested 60 compounds for their ability to kill human cancer cells.
“What was particularly exciting to us was to see, across various cancer cell lines, that some of them are quite potent,” Movassaghi says.
Lead author of the paper is MIT postdoc Nicolas Boyer. Other authors are MIT graduate student Justin Kim, UIUC chemistry professor Paul Hergenrother and UIUC graduate student Karen Morrison.
Many of the compounds tested in this study, known as epipolythiodiketopiperazine (ETP) alkaloids, are naturally produced by fungi. Scientists believe these compounds help fungi prevent other organisms from encroaching on their territory.
The compounds that kill cancer cells appear to be very selective, destroying them 1,000 times more effectively than they kill healthy blood cells.
The researchers also identified sections of the compounds that can be altered without discernably changing their activity. This is useful because it could allow chemists to use those points to attach the compounds to a delivery agent such as an antibody that would target them to cancer cells, without impairing their cancer-killing ability.
Larry Overman, a professor of chemistry at the University of California at Irvine, says the new study is an impressive advance.The research was funded by the National Institute of General Medical Sciences.
Source: http://web.mit.edu/newsoffice/2013/chemists-find-help-from-nature-in-fighting-cancer-0227.html
Innovative news from the world of technology. Objective is to keep a history of interesting new technology and see if it came to fruition.
Thursday, February 28, 2013
Tuesday, February 19, 2013
Indian Plant Compound Could Play Role In Cancer Cell Death
Gedunin, an extract of the Indian neem tree that has been used for centuries in Asia as a natural remedy to treat inflammation, fever, and malaria, may also be used to help kill cancer cells.
Cancer cells typically avoid death by hijacking molecular chaperones that guide and protect the proteins that ensure normal cellular function and then tricking them into helping mutated versions of those proteins stay alive, says Dr. Ahmed Chadli, a researcher at the GRU Cancer Center and senior author of the study.
Drug development has focused on the chaperone Hsp90 (heat shock protein 90) because it plays a key role in assisting mutated proteins, making it an attractive cancer drug target. But small molecules targeting Hsp90 have inadvertently resulted in the expression of proteins that protect cancer cells from programmed cell death, compromising the Hsp90 inhibitors in the clinic.
Chadli and his team found that gedunin attacks a co-chaperone, or helper protein, of Hsp90 called p23. Hence, gedunin leads to the inactivation of the Hsp90 machine and the killing of cancer cells without the production of anti-apoptotic proteins.
Source:
http://www.asianscientist.com/in-the-lab/gedunin-indian-plant-compound-cancer-cell-death-2013/
http://www.jbc.org/content/early/2013/01/25/jbc.M112.427328
Cancer cells typically avoid death by hijacking molecular chaperones that guide and protect the proteins that ensure normal cellular function and then tricking them into helping mutated versions of those proteins stay alive, says Dr. Ahmed Chadli, a researcher at the GRU Cancer Center and senior author of the study.
Drug development has focused on the chaperone Hsp90 (heat shock protein 90) because it plays a key role in assisting mutated proteins, making it an attractive cancer drug target. But small molecules targeting Hsp90 have inadvertently resulted in the expression of proteins that protect cancer cells from programmed cell death, compromising the Hsp90 inhibitors in the clinic.
Chadli and his team found that gedunin attacks a co-chaperone, or helper protein, of Hsp90 called p23. Hence, gedunin leads to the inactivation of the Hsp90 machine and the killing of cancer cells without the production of anti-apoptotic proteins.
Source:
http://www.asianscientist.com/in-the-lab/gedunin-indian-plant-compound-cancer-cell-death-2013/
http://www.jbc.org/content/early/2013/01/25/jbc.M112.427328
Friday, February 15, 2013
Nanoscale capsule kills cancer cells without harming healthy cells
A degradable nanoscale shell to carry proteins to cancer cells and stunt the growth of tumors without damaging healthy cells has been developed by a team led by researchers from the UCLA Henry Samueli School of Engineering and Applied Science.
The process does not present the risk of genetic mutation posed by gene therapies for cancer, or the risk to healthy cells caused by chemotherapy, which does not effectively discriminate between healthy and cancerous cells, said Yi Tang, a professor of chemical and biomolecular engineering and a member of the California NanoSystems Institute at UCLA.
The research was funded by the David and Lucille Packard Foundation and a breast cancer research grant from the Congressionally Directed Medical Research Program.
Source: http://www.kurzweilai.net/nanoscale-capsule-kills-cancer-cells-without-harming-healthy-cells
The process does not present the risk of genetic mutation posed by gene therapies for cancer, or the risk to healthy cells caused by chemotherapy, which does not effectively discriminate between healthy and cancerous cells, said Yi Tang, a professor of chemical and biomolecular engineering and a member of the California NanoSystems Institute at UCLA.
The research was funded by the David and Lucille Packard Foundation and a breast cancer research grant from the Congressionally Directed Medical Research Program.
Source: http://www.kurzweilai.net/nanoscale-capsule-kills-cancer-cells-without-harming-healthy-cells
Thursday, February 14, 2013
New world-record efficiency for thin-film silicon solar cells
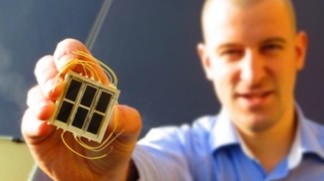 EPFL’s Institute of Microengineering has reached a remarkable 10.7% efficiency for a single-junction microcrystalline silicon solar cell, surpassing the previous world record of 10.1% held by the Japanese company Kaneka Corporation since 1998.
EPFL’s Institute of Microengineering has reached a remarkable 10.7% efficiency for a single-junction microcrystalline silicon solar cell, surpassing the previous world record of 10.1% held by the Japanese company Kaneka Corporation since 1998.The efficiency increase was also achieved with with only 1.8 microns of photovoltaic active material — 100 times less material than with standard wafer-based crystalline silicon PV technology.
Thin-film silicon technology indeed offers the advantages of saving up on raw material and offering low energy payback time, thus allowing module production prices as low as 35 €/m2 (47 $/m2), reaching the price level of standard roof tiles.
Work leading to this result was supported by the Swiss Federal Office of Energy (SFOE), the EU-FP7 program, the Swiss National Science Foundation (SNSF), and the Commission for Technology and Innovation (CTI).
Source: http://www.kurzweilai.net/new-world-record-efficiency-for-thin-film-silicon-solar-cells
Monday, February 11, 2013
Cancer battle: Scientists engineer new tumor-killing virus
A new genetically-engineered virus has been developed to kill cancer tumors and prevent the growth of new ones, according to a study. It was tested in 30 terminally-ill liver cancer patients and proved to significantly prolong their lives.
The study, which was recently published in the journal Nature Medicine, describes a four-week trial of the vaccine Pexa-Vec or JX-594 marking a step forward towards a successful treatment of solid tumors, AFP reports.
Sixteen out of 30 patients who were given a high dosage of therapy lived for 14.1 months on average, while the other 14 patients were given a low dosage and survived for 6.7 months.
"For the first time in medical history we have shown that a genetically-engineered virus can improve survival of cancer patients," study co-author David Kirn from California-based biotherapy company Jennerex told AFP.
The results of the study indicate that "Pexa-Vec treatment at both doses resulted in a reduction of tumor size and decreased blood flow to tumors," Jennerex said in a statement. “This is the first randomized clinical trial of an oncolytic immunotherapy demonstrating significantly prolonged overall survival.”
The new treatment uses oncolytic immunotherapy, which is a genetically modified type of virus that attacks tumors to induce a systemic immune response to cancer. It selectively replicates in tumor cells to achieve an antitumor effect.
The new virus "is designed to multiply in and subsequently destroy cancer cells, while at the same time making the patients' own immune defense system attack cancer cells also," added Kirn.
This trial shows concrete progress and proves that “Pexa-Vec treatment induces an immune response against the tumor."
Source: http://rt.com/news/new-virus-battles-cancer-888/
The study, which was recently published in the journal Nature Medicine, describes a four-week trial of the vaccine Pexa-Vec or JX-594 marking a step forward towards a successful treatment of solid tumors, AFP reports.
Sixteen out of 30 patients who were given a high dosage of therapy lived for 14.1 months on average, while the other 14 patients were given a low dosage and survived for 6.7 months.
"For the first time in medical history we have shown that a genetically-engineered virus can improve survival of cancer patients," study co-author David Kirn from California-based biotherapy company Jennerex told AFP.
The results of the study indicate that "Pexa-Vec treatment at both doses resulted in a reduction of tumor size and decreased blood flow to tumors," Jennerex said in a statement. “This is the first randomized clinical trial of an oncolytic immunotherapy demonstrating significantly prolonged overall survival.”
The new treatment uses oncolytic immunotherapy, which is a genetically modified type of virus that attacks tumors to induce a systemic immune response to cancer. It selectively replicates in tumor cells to achieve an antitumor effect.
The new virus "is designed to multiply in and subsequently destroy cancer cells, while at the same time making the patients' own immune defense system attack cancer cells also," added Kirn.
This trial shows concrete progress and proves that “Pexa-Vec treatment induces an immune response against the tumor."
Source: http://rt.com/news/new-virus-battles-cancer-888/
Tuesday, February 05, 2013
Some cancer mutations slow tumor growth
A typical cancer cell has thousands of mutations scattered throughout its genome and hundreds of mutated genes. However, only a handful of those genes, known as drivers, are responsible for cancerous traits such as uncontrolled growth. Cancer biologists have largely ignored the other mutations, believing they had little or no impact on cancer progression.
But a new study from MIT, Harvard University, the Broad Institute and Brigham and Women’s Hospital reveals, for the first time, that these so-called passenger mutations are not just along for the ride. When enough of them accumulate, they can slow or even halt tumor growth.
The findings, reported in this week’s Proceedings of the National Academy of Sciences, suggest that cancer should be viewed as an evolutionary process whose course is determined by a delicate balance between driver-propelled growth and the gradual buildup of passenger mutations that are damaging to cancer, says Leonid Mirny, an associate professor of physics and health sciences and technology at MIT and senior author of the paper.
In computer simulations, the researchers tested the possibility of treating tumors by boosting the impact of deleterious mutations. In their original simulation, each deleterious passenger mutation reduced the cell’s fitness by about 0.1 percent. When that was increased to 0.3 percent, tumors shrank under the load of their own mutations.
The same effect could be achieved in real tumors with drugs that interfere with proteins known as chaperones, Mirny suggests. After proteins are synthesized, they need to be folded into the correct shape, and chaperones help with that process. In cancerous cells, chaperones help proteins fold into the correct shape even when they are mutated, helping to suppress the effects of deleterious mutations.
Several potential drugs that inhibit chaperone proteins are now in clinical trials to treat cancer, although researchers had believed that they acted by suppressing the effects of driver mutations, not by enhancing the effects of passengers.
In current studies, the researchers are comparing cancer cell lines that have identical driver mutations but a different load of passenger mutations, to see which grow faster. They are also injecting the cancer cell lines into mice to see which are likeliest to metastasize.
The research was funded by the National Institutes of Health/National Cancer Institute Physical Sciences Oncology Center at MIT.
Source: http://web.mit.edu/newsoffice/2013/some-cancer-mutations-slow-tumor-growth-0204.html
But a new study from MIT, Harvard University, the Broad Institute and Brigham and Women’s Hospital reveals, for the first time, that these so-called passenger mutations are not just along for the ride. When enough of them accumulate, they can slow or even halt tumor growth.
The findings, reported in this week’s Proceedings of the National Academy of Sciences, suggest that cancer should be viewed as an evolutionary process whose course is determined by a delicate balance between driver-propelled growth and the gradual buildup of passenger mutations that are damaging to cancer, says Leonid Mirny, an associate professor of physics and health sciences and technology at MIT and senior author of the paper.
In computer simulations, the researchers tested the possibility of treating tumors by boosting the impact of deleterious mutations. In their original simulation, each deleterious passenger mutation reduced the cell’s fitness by about 0.1 percent. When that was increased to 0.3 percent, tumors shrank under the load of their own mutations.
The same effect could be achieved in real tumors with drugs that interfere with proteins known as chaperones, Mirny suggests. After proteins are synthesized, they need to be folded into the correct shape, and chaperones help with that process. In cancerous cells, chaperones help proteins fold into the correct shape even when they are mutated, helping to suppress the effects of deleterious mutations.
Several potential drugs that inhibit chaperone proteins are now in clinical trials to treat cancer, although researchers had believed that they acted by suppressing the effects of driver mutations, not by enhancing the effects of passengers.
In current studies, the researchers are comparing cancer cell lines that have identical driver mutations but a different load of passenger mutations, to see which grow faster. They are also injecting the cancer cell lines into mice to see which are likeliest to metastasize.
The research was funded by the National Institutes of Health/National Cancer Institute Physical Sciences Oncology Center at MIT.
Source: http://web.mit.edu/newsoffice/2013/some-cancer-mutations-slow-tumor-growth-0204.html
Monday, February 04, 2013
Mercedes engineers expect autonomous cars by 2020
German ingenieurs from Mercedes expect that by 2020 series models can at least partially drive themselves.
Source: http://www.zeit.de/auto/2013-01/auto-autonom
Saturday, February 02, 2013
Will we ever... grow synthetic organs in the lab?
Grow synthetic organs in the lab
Growing synthetic windpipes, artificial skin and replacement blood vessels is now a reality, but scientists are now turning their attention to their ultimate goal: growing new human kidneys or hearts.
In June 2011, an Eritrean man entered an operating theatre with a cancer-ridden windpipe, but left with a brand new one. People had received windpipe transplants before, but Andemariam Teklesenbet Beyene’s was different. His was the first organ of its kind to be completely grown in a lab using the patient's own cells.
The practicalities are, as you can imagine, less straightforward. Take the example I have already described. The process began with researchers taking 3D scans of Beyene’s windpipe, and from these scans Alexander Seifalian at University College London built an exact replica from a special polymer and a glass mould. This was flown to Sweden, where surgeon Paolo Macchiarini seeded this scaffold with stem cells taken from Beyene’s bone marrow. These stem cells, which can develop into every type of cell in the body, soaked into the structure and slowly recreated the man’s own tissues. The team at Stockholm’s Karolinska University Hospital incubated the growing windpipe in a bioreactor – a vat designed to mimic the conditions inside the human body.
Two days later, Macchiarini transplanted the windpipe during a 12-hour operation, and after a month, Beyene was discharged from the hospital, cancer-free. A few months later, the team repeated the trick with another cancer patient, an American man called Christopher Lyles.
“A good way to think about it is that there are four levels of complexity,” says Anthony Atala from the Wake Forest Institute for Regenerative Medicine, one of the leaders of the field. The first level includes flat organs like skin, which comprise just a few types of cells. Next up are tubes, like windpipes or blood vessels, with slightly more complex shapes and more varied collections of cells. The third level includes hollow sac-like organs, like the bladder or stomach. Unlike the tubes, which just act as pipes for fluid, these organs have to perform on demand – secreting, expanding or filtering as the situation arises.
Even after scientists successfully devise ways of growing organs, there are many logistical challenges to overcome before these isolated success stories can become everyday medical reality. “Can you manufacture them and grow them on large scales?” asks Robert Langer, a pioneer in the field. “Can you create them reproducibly? Can you preserve them [in the cold] so they have a reasonable shelf-life? There are a lot of very important engineering challenges to overcome.”
Source: http://www.bbc.com/future/story/20120223-will-we-ever-create-organs
Printing a human kidney
Surgeon Anthony Atala demonstrates an early-stage experiment that could someday solve the organ-donor problem: a 3D printer that uses living cells to output a transplantable kidney. Using similar technology, Dr. Atala's young patient Luke Massella received an engineered bladder 10 years ago.
Anthony Atala asks, "Can we grow organs instead of transplanting them?" His lab at the Wake Forest Institute for Regenerative Medicine is doing just that - engineering over 30 tissues and whole organs. Anthony Atala is the director of the Wake Forest Institute for Regenerative Medicine, where his work focuses on growing and regenerating tissues and organs. His team engineered the first lab-grown organ to be implanted into a human - a bladder - and is developing experimental fabrication technology that can "print" human tissue on demand.
In 2007, Atala and a team of Harvard University researchers showed that stem cells can be harvested from the amniotic fluid of pregnant women. This and other breakthroughs in the development of smart bio-materials and tissue fabrication technology promises to revolutionize the practice of medicine.
Source: http://www.bbc.com/future/story/20120621-printing-a-human-kidney
Growing synthetic windpipes, artificial skin and replacement blood vessels is now a reality, but scientists are now turning their attention to their ultimate goal: growing new human kidneys or hearts.
In June 2011, an Eritrean man entered an operating theatre with a cancer-ridden windpipe, but left with a brand new one. People had received windpipe transplants before, but Andemariam Teklesenbet Beyene’s was different. His was the first organ of its kind to be completely grown in a lab using the patient's own cells.
The practicalities are, as you can imagine, less straightforward. Take the example I have already described. The process began with researchers taking 3D scans of Beyene’s windpipe, and from these scans Alexander Seifalian at University College London built an exact replica from a special polymer and a glass mould. This was flown to Sweden, where surgeon Paolo Macchiarini seeded this scaffold with stem cells taken from Beyene’s bone marrow. These stem cells, which can develop into every type of cell in the body, soaked into the structure and slowly recreated the man’s own tissues. The team at Stockholm’s Karolinska University Hospital incubated the growing windpipe in a bioreactor – a vat designed to mimic the conditions inside the human body.
Two days later, Macchiarini transplanted the windpipe during a 12-hour operation, and after a month, Beyene was discharged from the hospital, cancer-free. A few months later, the team repeated the trick with another cancer patient, an American man called Christopher Lyles.
“A good way to think about it is that there are four levels of complexity,” says Anthony Atala from the Wake Forest Institute for Regenerative Medicine, one of the leaders of the field. The first level includes flat organs like skin, which comprise just a few types of cells. Next up are tubes, like windpipes or blood vessels, with slightly more complex shapes and more varied collections of cells. The third level includes hollow sac-like organs, like the bladder or stomach. Unlike the tubes, which just act as pipes for fluid, these organs have to perform on demand – secreting, expanding or filtering as the situation arises.
Even after scientists successfully devise ways of growing organs, there are many logistical challenges to overcome before these isolated success stories can become everyday medical reality. “Can you manufacture them and grow them on large scales?” asks Robert Langer, a pioneer in the field. “Can you create them reproducibly? Can you preserve them [in the cold] so they have a reasonable shelf-life? There are a lot of very important engineering challenges to overcome.”
Source: http://www.bbc.com/future/story/20120223-will-we-ever-create-organs
Printing a human kidney
Surgeon Anthony Atala demonstrates an early-stage experiment that could someday solve the organ-donor problem: a 3D printer that uses living cells to output a transplantable kidney. Using similar technology, Dr. Atala's young patient Luke Massella received an engineered bladder 10 years ago.
Anthony Atala asks, "Can we grow organs instead of transplanting them?" His lab at the Wake Forest Institute for Regenerative Medicine is doing just that - engineering over 30 tissues and whole organs. Anthony Atala is the director of the Wake Forest Institute for Regenerative Medicine, where his work focuses on growing and regenerating tissues and organs. His team engineered the first lab-grown organ to be implanted into a human - a bladder - and is developing experimental fabrication technology that can "print" human tissue on demand.
In 2007, Atala and a team of Harvard University researchers showed that stem cells can be harvested from the amniotic fluid of pregnant women. This and other breakthroughs in the development of smart bio-materials and tissue fabrication technology promises to revolutionize the practice of medicine.
Source: http://www.bbc.com/future/story/20120621-printing-a-human-kidney
Epigenetic reveal clues to ageing
Why do we develop wrinkles and why do our muscles waste away? Why do our brains and immune systems become less effective with time?
Prof Tim Spector, the author of a book on epigenetics, Identically Different, said: "There are epigenetic drugs in development, four for cancer. In terms of lifestyle, we know that exercise can switch off the main obesity genes epigenetically.
"Apart from stem cells, this is the hot area of ageing at the moment, finding ways of encouraging our genes to remain healthy is going to be a top priority in the next few years."
Source: http://www.bbc.co.uk/news/health-18400219
Epigenetics is all about changing the way our genes function by turning them off or making them more active.
Genes are the blueprint for building the human body. There's a copy of the whole blueprint in nearly every cell in the body, but clearly you don't need to use all of it all of the time. Bone cells will use different bits of the blueprint to nerve cells or light sensing cells in the eye.
Manel Esteller's team, at the Bellvitge Biomedical Research Institute, has shown that this control over the blueprint decays over time.
Adding small chemicals, methyl groups, to specific points of DNA is one of the main ways of turning a gene off.
Longer or healthier life?
It is possible to change a person's epigenome. Studies have already shown how a pregnant mother's diet can affect her child's risk of obesity epigenetically.
Prof Tim Spector, the author of a book on epigenetics, Identically Different, said: "There are epigenetic drugs in development, four for cancer. In terms of lifestyle, we know that exercise can switch off the main obesity genes epigenetically.
"Apart from stem cells, this is the hot area of ageing at the moment, finding ways of encouraging our genes to remain healthy is going to be a top priority in the next few years."
Source: http://www.bbc.co.uk/news/health-18400219
Tuesday, January 29, 2013
Mass cancer mapping centre opens
The devastating changes that turn healthy tissue into cancer are to be investigated in the biggest centre of its kind in the NHS.
The laboratories at the Institute of Cancer Research (ICR) will use information in tumour DNA to help find the best "personalised" treatments.
Its director said this was not science fiction and would be day-to-day practice in the NHS within a decade.
Rapid advances in being able to sequence the genetic code of patients are allowing breakthroughs in understanding which mutations transform a healthy cell into a cancerous one.
Identifying the mutations can then be used to choose the best treatment. The most famous example of this is the drug Herceptin, which is used in breast cancers with a certain genetic abnormality.
The new centre will test samples from patients at the Royal Marsden Hospital in London.
The ICR's director, Prof Alan Ashworth, said: "None of this is science fiction. This is now happening. We think we're pioneering the clinical application of this by setting up the Tumour Profiling Unit, but one would think this would be absolutely routine practice for every cancer patient - and that's what we're aiming to bring about."
Other challenges for the field include storing the data. The genetic codes of one million cancer patients would take up the same amount of space as YouTube.
Source: http://www.bbc.co.uk/news/health-21235103
The laboratories at the Institute of Cancer Research (ICR) will use information in tumour DNA to help find the best "personalised" treatments.
Its director said this was not science fiction and would be day-to-day practice in the NHS within a decade.
Rapid advances in being able to sequence the genetic code of patients are allowing breakthroughs in understanding which mutations transform a healthy cell into a cancerous one.
Identifying the mutations can then be used to choose the best treatment. The most famous example of this is the drug Herceptin, which is used in breast cancers with a certain genetic abnormality.
The new centre will test samples from patients at the Royal Marsden Hospital in London.
The ICR's director, Prof Alan Ashworth, said: "None of this is science fiction. This is now happening. We think we're pioneering the clinical application of this by setting up the Tumour Profiling Unit, but one would think this would be absolutely routine practice for every cancer patient - and that's what we're aiming to bring about."
Other challenges for the field include storing the data. The genetic codes of one million cancer patients would take up the same amount of space as YouTube.
Source: http://www.bbc.co.uk/news/health-21235103
Monday, January 21, 2013
Leprosy bacteria use 'biological alchemy'
Infectious bacteria have for the first time been caught performing "biological alchemy" to transform parts of a host body into those more suited to their purposes, by a team in Edinburgh.
The study, in the journal Cell, showed leprosy-causing bacteria turning nerves into stem cells and muscle.
The authors said the "clever and sophisticated" technique could further therapies and stem-cell research.
Prof Rambukkana also believes it is "probable" that other species of bacteria would have evolved the same ability to reprogramme their host.
Prof Chris Mason, a specialist in stem cell research at University College London, said: "The ability of bacteria to convert one mammalian cell type to another is 'alchemy' by nature on a grand scale.
"The next essential step is to translate this valuable piece of knowledge into tangible benefits for patients - a process that may take a decade before its relevance to clinical medicine is fully understood."
Prof Diana Lockwood, from the London School of Hygiene and Tropical Medicine, said: "Their finding that bacteria can reprogramme cells is very interesting and exciting."
Dr Rob Buckle, head of regenerative medicine at the Medical Research Council, said: "This discovery is important not just for our understanding and treatment of bacterial disease, but for the rapidly progressing field of regenerative medicine."
Source: http://www.bbc.co.uk/news/health-21056644
The study, in the journal Cell, showed leprosy-causing bacteria turning nerves into stem cells and muscle.
The authors said the "clever and sophisticated" technique could further therapies and stem-cell research.
Prof Rambukkana also believes it is "probable" that other species of bacteria would have evolved the same ability to reprogramme their host.
Prof Chris Mason, a specialist in stem cell research at University College London, said: "The ability of bacteria to convert one mammalian cell type to another is 'alchemy' by nature on a grand scale.
"The next essential step is to translate this valuable piece of knowledge into tangible benefits for patients - a process that may take a decade before its relevance to clinical medicine is fully understood."
Prof Diana Lockwood, from the London School of Hygiene and Tropical Medicine, said: "Their finding that bacteria can reprogramme cells is very interesting and exciting."
Dr Rob Buckle, head of regenerative medicine at the Medical Research Council, said: "This discovery is important not just for our understanding and treatment of bacterial disease, but for the rapidly progressing field of regenerative medicine."
Source: http://www.bbc.co.uk/news/health-21056644
Wednesday, January 16, 2013
Healing Blind Mice
Blind mice can see again, after researchers transplanted developing cells into their eyes and found they could reform the entire light-sensitive layer of the retina.
Study was led by Dr. Mandeep Singh, an eye surgeon from the National University Hospital of Singapore and a clinician-scientist with the Singapore Eye Research Institute (SERI), while he was a Ph.D. student with Professor Robert MacLaren at the University of Oxford, U.K.
The researchers worked with mice that were blind due to complete loss of the light-sensing photoreceptor cells in their retinas. This is the most relevant mouse model for treating patients who are blind from retinitis pigmentosa.
The article can be found at: Singh M et al. (2013) Reversal of end-stage retinal degeneration and restoration of visual function by photoreceptor transplantation.
Source: http://www.asianscientist.com/in-the-lab/healing-blind-mice-2013/
Study was led by Dr. Mandeep Singh, an eye surgeon from the National University Hospital of Singapore and a clinician-scientist with the Singapore Eye Research Institute (SERI), while he was a Ph.D. student with Professor Robert MacLaren at the University of Oxford, U.K.
The researchers worked with mice that were blind due to complete loss of the light-sensing photoreceptor cells in their retinas. This is the most relevant mouse model for treating patients who are blind from retinitis pigmentosa.
The article can be found at: Singh M et al. (2013) Reversal of end-stage retinal degeneration and restoration of visual function by photoreceptor transplantation.
Source: http://www.asianscientist.com/in-the-lab/healing-blind-mice-2013/
Audi’s Cars Can Now Park Themselves; Driving Themselves Is Not Far Behind
Move over, Google. Audi just became the second company to be licensed to run autonomous vehicles in Nevada. That means the company can now test its autonomous vehicles on the state’s public roads.
Volkswagen Group works on innovative technologies, like advanced driver assistance, navigation, and of course, piloted driving (Audi prefers the term "piloted" to "autonomous" because it implies that the human in the car still has ultimate responsibility).
Audi representatives say that piloted parking will be commercialized in the next few years. Autonomous vehicles could be available by the end of the decade. In the coming years, automakers will take baby steps towards producing fully autonomous vehicles, starting with piloted parking technology. By the time self-driving cars hit the road, they won’t seem so sci-fi.
Source: http://www.fastcoexist.com/1681188/audis-cars-can-now-park-themselves-driving-themselves-is-not-far-behind?utm_source=feedburner&utm_medium=feed&utm_campaign=Feed%3A+fastcompany%2Fheadlines+(Fast+Company)#1
Volkswagen Group works on innovative technologies, like advanced driver assistance, navigation, and of course, piloted driving (Audi prefers the term "piloted" to "autonomous" because it implies that the human in the car still has ultimate responsibility).
Audi representatives say that piloted parking will be commercialized in the next few years. Autonomous vehicles could be available by the end of the decade. In the coming years, automakers will take baby steps towards producing fully autonomous vehicles, starting with piloted parking technology. By the time self-driving cars hit the road, they won’t seem so sci-fi.
Source: http://www.fastcoexist.com/1681188/audis-cars-can-now-park-themselves-driving-themselves-is-not-far-behind?utm_source=feedburner&utm_medium=feed&utm_campaign=Feed%3A+fastcompany%2Fheadlines+(Fast+Company)#1
Thursday, January 10, 2013
'Drug holidays' beat cancer drug resistance in mice
Introducing medication-free spells to some cancer treatments may keep patients alive for longer, studies in mice with skin cancer suggest.
The animals had melanoma, which can rapidly become resistant to treatments.
However, a study in the journal Nature showed tumours also became dependent on the drug to survive. Withdrawing treatment caused tumours to shrink.
Experts said the findings were exciting, but still needed testing in people.
The tumours gain resistance by changing the chemistry of the inside of a cell. However, the researchers showed this process left the cancer cells dependent on the drug - like an addict.
When the mice were no longer given the drug, the tumours began to shrink.
The scientists used this knowledge to test a new way of prescribing the medication. Instead of giving the drug every day, the mice were given drugs for four weeks and then had a two week "drug holiday" before starting the pattern over again.
Efim Guzik, professor of cancer biology at University of California, San Francisco, said: "Remarkably, intermittent dosing with vemurafenib prolonged the lives of mice with drug-resistant melanoma tumours.
Whether the same effect would be seen in people given the same medication is uncertain.
Prof Mark Middleton, director of Cancer Research UK's Experimental Cancer Medicine Centre in Oxford, said: "We still need to test the idea in the clinic, but these results suggest a way in which this important new treatment might be able to increase the benefit to patients and their families.
Prof Marais said the same effect is possible in other forms of targeted cancer drug treatment.
Source: http://www.bbc.co.uk/news/health-20956179
The animals had melanoma, which can rapidly become resistant to treatments.
However, a study in the journal Nature showed tumours also became dependent on the drug to survive. Withdrawing treatment caused tumours to shrink.
Experts said the findings were exciting, but still needed testing in people.
The tumours gain resistance by changing the chemistry of the inside of a cell. However, the researchers showed this process left the cancer cells dependent on the drug - like an addict.
When the mice were no longer given the drug, the tumours began to shrink.
The scientists used this knowledge to test a new way of prescribing the medication. Instead of giving the drug every day, the mice were given drugs for four weeks and then had a two week "drug holiday" before starting the pattern over again.
Efim Guzik, professor of cancer biology at University of California, San Francisco, said: "Remarkably, intermittent dosing with vemurafenib prolonged the lives of mice with drug-resistant melanoma tumours.
Whether the same effect would be seen in people given the same medication is uncertain.
Prof Mark Middleton, director of Cancer Research UK's Experimental Cancer Medicine Centre in Oxford, said: "We still need to test the idea in the clinic, but these results suggest a way in which this important new treatment might be able to increase the benefit to patients and their families.
Prof Marais said the same effect is possible in other forms of targeted cancer drug treatment.
Source: http://www.bbc.co.uk/news/health-20956179
Sickle-shaped blood cells 'may kill cancer cells in mice'
Misshapen red blood cells could be used as a tool to kill cancer cells in mice, research in the journal Plos One shows.
Sickle-shaped cells can stick together in blood vessels surrounding tumours in mice and block blood flowing to the cancer, researchers says.
The irregularly shaped cells can also deposit toxic residues on the tumour, leading to cancer cell death.
The US researchers from Duke University and Jenomic, a private research company, gave a fluorescent sickle-cell solution to mice with cancer and watched what happened inside their systems.
Within five minutes the misshapen cells began to stick like 'Velcro' to blood vessels near the oxygen-starved areas of the tumour, Prof Mark Dewhirst co-author of the study, from Duke University, said.
"We found that sickle cells show a highly unique natural attraction to oxygen-deprived tumours.
"Once clustered within the tumour, the sickle cells deposit a toxic residue... causing tumour cell death," Dr David Terman, a co-author of the study and head of molecular genetics at Jenomic said.
"This is an intriguing new tactic for destroying tumours that are resistant to standard treatments, but the research was carried out in mice so the next challenge will be to show whether this approach is safe and effective in people with cancer," said Dr Emma Smith of Cancer Research UK.
The researchers say their approach could be directed at breast cancers, prostate cancers and many other tumours that develop resistance to current therapies, once more animal studies and human trials have been carried out.
Source: http://www.bbc.co.uk/news/health-20959968
Sickle-shaped cells can stick together in blood vessels surrounding tumours in mice and block blood flowing to the cancer, researchers says.
The irregularly shaped cells can also deposit toxic residues on the tumour, leading to cancer cell death.
The US researchers from Duke University and Jenomic, a private research company, gave a fluorescent sickle-cell solution to mice with cancer and watched what happened inside their systems.
Within five minutes the misshapen cells began to stick like 'Velcro' to blood vessels near the oxygen-starved areas of the tumour, Prof Mark Dewhirst co-author of the study, from Duke University, said.
"We found that sickle cells show a highly unique natural attraction to oxygen-deprived tumours.
"Once clustered within the tumour, the sickle cells deposit a toxic residue... causing tumour cell death," Dr David Terman, a co-author of the study and head of molecular genetics at Jenomic said.
"This is an intriguing new tactic for destroying tumours that are resistant to standard treatments, but the research was carried out in mice so the next challenge will be to show whether this approach is safe and effective in people with cancer," said Dr Emma Smith of Cancer Research UK.
The researchers say their approach could be directed at breast cancers, prostate cancers and many other tumours that develop resistance to current therapies, once more animal studies and human trials have been carried out.
Source: http://www.bbc.co.uk/news/health-20959968
Friday, January 04, 2013
The Future of Medicine Is Now
- Surgeons at Boston Children’s Hospital have developed a way to help children born with half a heart to essentially grow a whole one — by marshaling the body’s natural capacity to heal and develop.
- Oxford Nanopore Technologies has unveiled the first of a generation of tiny DNA sequencing devices that many predict will eventually be as ubiquitous as cellphones — it’s already the size of one.
- A test developed by Foundation Medicine Inc. enables doctors to test a tumor sample for 280 different genetic mutations suspected of driving tumor growth.
- Last month, the FDA cleared a new iPhone add-on that lets doctors take an electrocardiogram just about anywhere. Other smartphone apps help radiologists read medical images and allow patients to track moles for signs of skin cancer.
- Gene therapy is poised to become a viable option for a variety of often life-threatening medical conditions, especially those resulting from a single defective gene.

Source:
Unleash an army of immune cells to hunt down a cancer
MK3475, being developed by Merck & Co., is among a new category of drugs that unleash an army of immune cells to hunt down a cancer.
For decades, cancer researchers have wondered why the immune system typically doesn't treat tumor cells as invaders and target them. Part of the mystery was recently solved: Tumors protect themselves by hijacking the body's natural brake for the immune system.
MK3475, being developed by Merck & Co., is among a new category of drugs that release the brake, unleashing an army of immune cells to hunt down the cancer. A recent report from a trial in which Mr. Stutz participated said that of 85 patients who took the drug, 51% saw their tumors significantly shrink; in eight cases, the tumors couldn't be detected on imaging tests.
Still, not everyone was helped. And unleashing the immune system can put normal cells in harm's way: In studies of MK3745 and similar drugs, some patients developed serious side effects related to immune-system response, including a small number who died.
Source:
http://online.wsj.com/article/SB10001424127887323530404578205692226506324.html
http://www.mercknewsroom.com/press-release/research-and-development-news/merck-presents-early-stage-interim-data-mk-3475-investig
For decades, cancer researchers have wondered why the immune system typically doesn't treat tumor cells as invaders and target them. Part of the mystery was recently solved: Tumors protect themselves by hijacking the body's natural brake for the immune system.
MK3475, being developed by Merck & Co., is among a new category of drugs that release the brake, unleashing an army of immune cells to hunt down the cancer. A recent report from a trial in which Mr. Stutz participated said that of 85 patients who took the drug, 51% saw their tumors significantly shrink; in eight cases, the tumors couldn't be detected on imaging tests.
Still, not everyone was helped. And unleashing the immune system can put normal cells in harm's way: In studies of MK3745 and similar drugs, some patients developed serious side effects related to immune-system response, including a small number who died.
Source:
http://online.wsj.com/article/SB10001424127887323530404578205692226506324.html
http://www.mercknewsroom.com/press-release/research-and-development-news/merck-presents-early-stage-interim-data-mk-3475-investig
Immune system 'booster' may hit cancer
Vast numbers of cells that can attack cancer and HIV have been grown in the lab, and could potentially be used to fight disease.
The cells naturally occur in small numbers, but it is hoped injecting huge quantities back into a patient could turbo-charge the immune system.
The Japanese research is published in the journal Cell Stem Cell.
The researchers concentrated on a type of white blood cell known as a cytotoxic T-cell, which can recognise telltale markings of infection or cancer on the surfaces of cells. If a marking is recognised, it launches an attack.
Teams at the University of Tokyo and the Riken Research Centre for Allergy and Immunology used advances in stem cell technology to make more T-cells.
Dr Hiroshi Kawamoto, who worked on the cancer immune cells at Riken, said: "The next step will be to test whether these T-cells can selectively kill tumour cells, but not other cells in the body.
"If they do, these cells might be directly injected into patients for therapy. This could be realized in the not-so-distant future."
Dr Hiromitsu Nakauchi from the University of Tokyo said it was "unclear" whether this technique would help in treating HIV and that other infections and cancer may be a better place to start.
Prof Alan Clarke, the director of the European Cancer Stem Cell Research Institute at Cardiff University, said: "This is a potentially very exciting development which extends our capacity to develop novel cell therapies."
Prof Sir John Burn, from the Institute of Genetic Medicine at Newcastle University, said: "This is a very appealing concept and the research team are to be congratulated on demonstrating the feasibility of expanding these killer cells.
Source: http://www.bbc.co.uk/news/health-20898931
The cells naturally occur in small numbers, but it is hoped injecting huge quantities back into a patient could turbo-charge the immune system.
The Japanese research is published in the journal Cell Stem Cell.
The researchers concentrated on a type of white blood cell known as a cytotoxic T-cell, which can recognise telltale markings of infection or cancer on the surfaces of cells. If a marking is recognised, it launches an attack.
Teams at the University of Tokyo and the Riken Research Centre for Allergy and Immunology used advances in stem cell technology to make more T-cells.
Dr Hiroshi Kawamoto, who worked on the cancer immune cells at Riken, said: "The next step will be to test whether these T-cells can selectively kill tumour cells, but not other cells in the body.
"If they do, these cells might be directly injected into patients for therapy. This could be realized in the not-so-distant future."
Dr Hiromitsu Nakauchi from the University of Tokyo said it was "unclear" whether this technique would help in treating HIV and that other infections and cancer may be a better place to start.
Prof Alan Clarke, the director of the European Cancer Stem Cell Research Institute at Cardiff University, said: "This is a potentially very exciting development which extends our capacity to develop novel cell therapies."
Prof Sir John Burn, from the Institute of Genetic Medicine at Newcastle University, said: "This is a very appealing concept and the research team are to be congratulated on demonstrating the feasibility of expanding these killer cells.
Source: http://www.bbc.co.uk/news/health-20898931
Thursday, January 03, 2013
Friday, December 21, 2012
Trojan-horse therapy 'completely eliminates' cancer in mice
An experimental "Trojan-horse" cancer therapy has completely eliminated prostate cancer in experiments on mice, according to UK researchers.
The team hid cancer killing viruses inside the immune system in order to sneak them into a tumour.
Once inside, a study in the journal Cancer Research showed, tens of thousands of viruses were released to kill the cancerous cells.
Using viruses to destroy rapidly growing tumours is an emerging field in cancer therapy, however one of the challenges is getting the viruses deep inside the tumour where they can do the damage.
"The problem is penetration," Prof Claire Lewis from the University of Sheffield told the BBC. She leads a team which uses white blood cells as 'Trojan horses' to deliver the viral punch.
Dr Kate Holmes, head of research at Prostate Cancer UK, said: "It demonstrates that this innovative method of delivering a tumour-killing virus direct to the cancer site is successful at reducing the development of advanced prostate tumours which have been treated with chemotherapy and radiotherapy.
"If this treatment goes on to be successful in human trials, it could mark substantial progress in finding better treatments for men with prostate cancer which has spread to the bone."
Source: http://www.bbc.co.uk/news/health-20795977
The team hid cancer killing viruses inside the immune system in order to sneak them into a tumour.
Once inside, a study in the journal Cancer Research showed, tens of thousands of viruses were released to kill the cancerous cells.
Using viruses to destroy rapidly growing tumours is an emerging field in cancer therapy, however one of the challenges is getting the viruses deep inside the tumour where they can do the damage.
"The problem is penetration," Prof Claire Lewis from the University of Sheffield told the BBC. She leads a team which uses white blood cells as 'Trojan horses' to deliver the viral punch.
Dr Kate Holmes, head of research at Prostate Cancer UK, said: "It demonstrates that this innovative method of delivering a tumour-killing virus direct to the cancer site is successful at reducing the development of advanced prostate tumours which have been treated with chemotherapy and radiotherapy.
"If this treatment goes on to be successful in human trials, it could mark substantial progress in finding better treatments for men with prostate cancer which has spread to the bone."
Source: http://www.bbc.co.uk/news/health-20795977
Subscribe to:
Posts (Atom)





